How to Create an Efficient Medical Billing Workflow
Medical Billing
Medical Billing
Medical billing is the backbone of any healthcare practice’s financial health. An inefficient billing workflow can lead to delayed payments, increased claim denials, and unnecessary administrative burden that ultimately affects both patient care and practice profitability. Creating a streamlined, efficient medical billing workflow is essential for maintaining a thriving healthcare practice in today’s complex healthcare landscape.

The medical billing process involves multiple steps, from patient registration to final payment collection, and each stage presents opportunities for optimization. When done correctly, an efficient billing workflow reduces errors, accelerates payment cycles, and ensures compliance with ever-changing healthcare regulations. This comprehensive guide will walk you through the essential components of creating a medical billing workflow that maximizes efficiency while minimizing errors and delays.
Understanding the Medical Billing Cycle
Before diving into workflow optimization, it’s crucial to understand the complete medical billing cycle. This process typically begins when a patient schedules an appointment and continues until the final payment is collected. The cycle includes patient registration, insurance verification, service documentation, claim submission, payment processing, and follow-up on outstanding accounts.
Each step in this cycle is interconnected, meaning inefficiencies in one area inevitably impact the entire process. For instance, incomplete patient registration can lead to claim denials, while poor documentation practices can result in delayed payments or compliance issues. Understanding these connections is the first step toward creating a more efficient workflow.
The modern medical billing environment also requires practices to navigate complex insurance requirements, coding updates, and regulatory changes. An efficient workflow must be flexible enough to adapt to these changes while maintaining consistency in core processes. This balance between adaptability and standardization is key to long-term success.
Step 1: Optimize Patient Registration and Data Collection
The foundation of efficient medical billing begins with accurate patient registration. This initial step sets the tone for the entire billing process, and errors here can cascade through every subsequent stage. Implementing a robust registration system that captures complete and accurate patient information is essential for reducing downstream billing issues.
Start by creating standardized registration forms that collect all necessary demographic information, insurance details, and authorization signatures. Digital registration systems can significantly improve accuracy by using validation rules, dropdown menus, and required fields that prevent incomplete submissions. These systems can also integrate with insurance verification tools to check coverage in real-time.
Training front-desk staff on proper registration procedures is equally important. Staff should understand the importance of collecting complete information and be equipped to handle common registration challenges. Regular training sessions on insurance requirements, HIPAA compliance, and data entry best practices help maintain high standards.
Consider implementing pre-registration processes for scheduled appointments. Allowing patients to complete registration online before their visit reduces wait times and gives staff more opportunity to verify information accuracy. This proactive approach also enables early identification of insurance issues that might affect the visit.
Step 2: Medical Billing
Insurance verification is a critical component that can make or break your billing efficiency. Verifying patient coverage, benefits, and authorization requirements before services are rendered prevents claim denials and reduces payment delays. An effective verification process should be systematic, thorough, and conducted well in advance of patient visits.
Establish a dedicated timeframe for insurance verification, ideally 24-48 hours before scheduled appointments. This allows sufficient time to resolve any issues and communicate with patients about coverage limitations or required authorizations. Create verification checklists that ensure consistent coverage of all necessary elements, including eligibility, benefits, copayments, deductibles, and prior authorization requirements.
Technology can significantly streamline verification processes. Many practice management systems offer automated eligibility checking that can verify coverage and benefits electronically. These systems can flag potential issues and generate alerts for staff attention. However, automated systems should be supplemented with manual verification for complex cases or when dealing with less common insurance plans.
Document all verification activities thoroughly. Maintain records of verification dates, staff members responsible, and any special instructions or limitations discovered. This documentation becomes invaluable when addressing claim issues or patient billing questions later in the process.
Step 3: Establish Clear Documentation Standards
Accurate and complete documentation is essential for successful claim processing and compliance with healthcare regulations. Poor documentation is one of the leading causes of claim denials and audit failures. Establishing clear documentation standards and ensuring consistent adherence across all providers and staff is crucial for billing efficiency.
Develop comprehensive documentation guidelines that cover all aspects of patient encounters. These guidelines should specify required elements for different types of visits, procedures, and diagnoses. Include templates and examples that help providers understand expectations and maintain consistency. Regular training on documentation requirements helps ensure ongoing compliance.
Implement quality assurance processes to review documentation before claim submission. This might include peer reviews, supervisor audits, or automated screening tools that flag potential issues. Catching documentation problems early prevents claim denials and reduces the need for costly appeals or resubmissions.
Consider the timing of documentation completion. Encourage providers to complete notes and coding promptly after patient encounters while details are fresh. Delayed documentation often results in incomplete or inaccurate records that can impact billing success. Some practices implement documentation deadlines or use technology reminders to encourage timely completion.
Step 4: Streamline Coding and Charge Entry
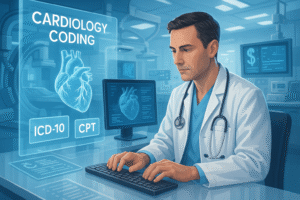
Accurate medical coding is fundamental to successful billing. Errors in procedure codes, diagnosis codes, or charge entry can result in claim denials, delayed payments, or compliance issues. Creating a streamlined coding and charge entry process reduces errors while improving efficiency.
Invest in ongoing coding education for all relevant staff. Medical coding is complex and constantly evolving, with regular updates to CPT, ICD-10, and HCPCS codes. Regular training ensures staff stay current with coding changes and understand proper application of codes to different scenarios. Consider certification programs or continuing education opportunities that enhance coding expertise.
Implement coding audits and quality checks as part of your routine workflow. Regular audits help identify patterns of coding errors and provide opportunities for targeted education. Some practices use coding software that includes built-in edits and alerts to catch potential errors before claim submission.

Establish clear procedures for charge entry, including timeframes for completion and quality control measures. Charges should be entered promptly and accurately, with appropriate review processes to catch errors. Consider using electronic charge capture systems that integrate with your EHR and practice management system to reduce manual entry errors.
Step 5: Optimize Claim Submission and Management
Efficient claim submission processes ensure that clean claims are submitted promptly and accurately. The goal is to achieve high first-pass claim acceptance rates while minimizing the time between service delivery and claim submission. This requires attention to both technical processes and workflow management.
Establish regular claim submission schedules that balance efficiency with cash flow needs. Daily claim submission is often optimal, ensuring prompt payment while allowing time for quality review. Batch processing can improve efficiency, but avoid delays that unnecessarily extend payment cycles.
Implement claim scrubbing technology that identifies potential errors before submission. These systems can catch common errors like missing or invalid codes, demographic mismatches, or authorization issues. While not perfect, claim scrubbing significantly reduces denial rates and improves first-pass acceptance.
Monitor key performance indicators related to claim submission, including submission timeframes, first-pass acceptance rates, and denial patterns. Regular monitoring helps identify process improvements and ensures consistent performance. Share these metrics with staff to maintain focus on quality and efficiency.
Step 6: Develop Effective Denial Management
Even with the best processes, some claim denials are inevitable. An efficient denial management workflow minimizes the impact of denials on cash flow and prevents them from becoming write-offs. Effective denial management requires prompt identification, systematic analysis, and appropriate corrective action.
Implement daily denial review processes that categorize denials by type and priority. Some denials require immediate attention, while others can be addressed systematically over time. Develop standard procedures for common denial types, including step-by-step instructions for resolution.
Track denial patterns to identify systematic issues that can be addressed proactively. If certain procedure codes consistently generate denials, investigate whether the issue stems from coding errors, documentation problems, or payer policy changes. Addressing root causes prevents future denials and improves overall efficiency.
Establish timeframes for denial resolution and monitor compliance with these standards. Aged denials become increasingly difficult to resolve and may eventually become uncollectable. Prompt attention to denials maximizes recovery potential and maintains healthy accounts receivable.
Step 7: Implement Patient Payment Processes
Patient financial responsibility has increased significantly in recent years, making effective patient payment processes essential for practice financial health. An efficient workflow should address patient communication, payment options, and collection procedures in a coordinated manner.
Develop clear patient communication strategies that explain financial responsibilities before, during, and after service delivery. Patients should understand their obligations, available payment options, and consequences of non-payment. Clear communication reduces confusion and improves collection rates.
Offer multiple payment options to accommodate different patient preferences and financial situations. This might include online payment portals, payment plans, credit card processing, and automatic payment options. The easier you make it for patients to pay, the more likely they are to do so promptly.
Implement systematic follow-up procedures for outstanding patient balances. This should include automated statements, phone calls, and eventually collection agency referrals for appropriate accounts. Consistency in follow-up efforts improves collection rates and demonstrates the practice’s commitment to collecting earned revenue.
Technology Integration and Automation
Modern medical billing workflows benefit significantly from technology integration and automation. The right technology can reduce manual work, minimize errors, and improve overall efficiency. However, successful technology implementation requires careful planning and ongoing management.
Practice management systems serve as the foundation for efficient billing workflows. These systems should integrate seamlessly with EHR systems, billing software, and other practice technologies. Look for systems that offer automated features like eligibility checking, claim scrubbing, and payment posting.
Consider robotic process automation (RPA) for repetitive tasks like prior authorization processing, claim status checking, and payment posting. RPA can handle high-volume, routine tasks more efficiently than manual processes while freeing staff to focus on complex issues requiring human judgment.
Implement business intelligence tools that provide insights into billing performance and identify improvement opportunities. These tools can analyze patterns in denials, payment delays, and staff productivity to guide workflow optimization efforts.
Monitoring and Continuous Improvement
Creating an efficient medical billing workflow is not a one-time project but an ongoing process of monitoring, analysis, and improvement. Regular assessment of workflow performance helps identify areas for enhancement and ensures continued efficiency as circumstances change.
Establish key performance indicators (KPIs) that measure important aspects of billing performance. These might include days in accounts receivable, first-pass claim acceptance rates, denial rates, and collection percentages. Regular monitoring of these metrics provides objective measures of workflow efficiency.
Conduct regular staff meetings to discuss billing performance, identify challenges, and gather improvement suggestions. Front-line staff often have valuable insights into workflow inefficiencies and practical solutions. Creating an environment where staff feel comfortable suggesting improvements can lead to significant enhancements.
Stay informed about industry changes that might affect your billing workflow. This includes regulatory updates, payer policy changes, and new technology options. Proactive adaptation to industry changes helps maintain efficiency and avoid disruptions.
Conclusion
Creating an efficient medical billing workflow requires attention to every aspect of the billing process, from initial patient registration through final payment collection. Success depends on establishing clear procedures, implementing appropriate technology, training staff effectively, and maintaining focus on continuous improvement.
The investment in workflow optimization pays dividends through improved cash flow, reduced administrative burden, and enhanced compliance with healthcare regulations. While the initial effort required to establish efficient processes may seem substantial, the long-term benefits to practice operations and financial health make this investment essential.
Remember that workflow efficiency is not just about speed but also about accuracy, compliance, and patient satisfaction. The best billing workflows balance efficiency with quality, ensuring that the pursuit of faster processing doesn’t compromise the accuracy and professionalism that patients and payers expect.
By following the guidelines outlined in this article and maintaining commitment to ongoing improvement, healthcare practices can create billing workflows that support both financial success and excellent patient care. The result is a more sustainable practice that can thrive in the challenging healthcare environment while providing the resources necessary for continued growth and development.



