How to Reduce Patient Billing Complaints: A Comprehensive Guide
Patient Billing Complaints
Patient Billing Complaints
Patient billing complaints represent one of the most significant sources of dissatisfaction in healthcare, often overshadowing the quality of medical care provided. These complaints can damage patient relationships, harm an organization’s reputation, and create substantial administrative burdens. Understanding the root causes and implementing systematic solutions is essential for healthcare providers who want to maintain patient trust while ensuring financial sustainability.

Understanding the Root Causes of Billing Complaints
The foundation of reducing billing complaints lies in understanding why they occur. Most billing disputes stem from a lack of transparency and communication rather than actual billing errors. Patients frequently receive bills weeks or months after treatment, with little context about what services were provided or why certain charges apply. The complexity of medical billing, combined with insurance processes that patients don’t fully understand, creates an environment ripe for confusion and frustration.
Common triggers include unexpected charges that weren’t discussed before treatment, bills that arrive long after the service date, confusing medical terminology on statements, and discrepancies between what patients expected to pay and their actual financial responsibility. Insurance-related issues, such as denied claims or changes in coverage that patients weren’t aware of, also generate significant complaints. Additionally, poor customer service experiences when patients attempt to resolve billing questions can escalate minor concerns into major complaints.
Establishing Transparent Communication Practices
Proactive communication serves as the most effective tool for preventing billing complaints. This begins with clear, upfront discussions about costs before treatment whenever possible. Staff should be trained to explain estimated costs, insurance coverage limitations, and potential out-of-pocket expenses in simple, understandable terms. Written estimates should accompany verbal explanations, giving patients documentation they can reference later.
Patient education plays a crucial role in this process. Many patients don’t understand basic insurance concepts like deductibles, copayments, and coinsurance. Healthcare organizations should develop educational materials that explain these concepts in plain language, along with information about their specific billing processes and payment policies. Regular communication during the billing cycle, including status updates on insurance processing and explanations of any delays, helps maintain transparency and reduces anxiety.
When bills are sent, they should include clear explanations of services provided, dates of service, and detailed breakdowns of charges. Avoid medical jargon and codes without explanation. Include contact information for billing questions and encourage patients to call with any concerns before the bill becomes overdue.
Implementing Effective Staff Training Programs
Front-line staff members are often the first point of contact for billing-related concerns, making their training critical to complaint reduction. Comprehensive training programs should cover both technical billing knowledge and customer service skills. Staff need to understand insurance processes, common billing scenarios, and how to explain complex financial concepts in accessible language.
Training should emphasize empathy and active listening skills. When patients express frustration about billing issues, staff responses can either defuse or escalate the situation. Teaching staff to acknowledge patient concerns, ask clarifying questions, and work collaboratively toward solutions creates positive interactions even when addressing problems.
Regular refresher training sessions help staff stay current with changing insurance regulations, new billing procedures, and evolving best practices. Role-playing exercises can help staff practice handling difficult conversations and develop confidence in addressing various billing scenarios.
Optimizing Billing Processes and Technology
Modern billing software and technology solutions can significantly reduce errors and improve efficiency. Automated systems can catch common mistakes before bills are sent, reducing the likelihood of complaints related to billing errors. Electronic health records integration ensures that billing reflects actual services provided, minimizing discrepancies.
Patient portals provide convenient access to billing information, allowing patients to view statements, track insurance processing, and make payments online. These self-service options reduce the volume of billing inquiries while giving patients more control over their billing experience. Mobile-friendly interfaces are particularly important, as many patients prefer to handle financial matters using their smartphones.
Regular audits of billing processes help identify recurring issues and opportunities for improvement. Analyzing complaint patterns can reveal systemic problems that need attention, such as particular types of charges that consistently generate questions or specific insurance processes that create confusion.
Developing Comprehensive Financial Policies
Clear, well-communicated financial policies provide structure for both staff and patients. These policies should cover payment expectations, financial assistance programs, payment plan options, and procedures for handling billing disputes. Policies should be written in plain language and made easily accessible to patients through websites, patient portals, and printed materials.
Financial hardship policies are particularly important, as many billing complaints stem from patients’ inability to pay rather than disagreement with charges. Offering payment plans, sliding-scale fees, or charity care programs can prevent complaints while ensuring that financial constraints don’t prevent patients from receiving necessary care. Clear eligibility criteria and application processes help both staff and patients understand available options.
Collection policies should balance the need to collect payment with maintaining positive patient relationships. Aggressive collection practices often generate complaints and can damage an organization’s reputation. Graduated approaches that start with gentle reminders and progress to more assertive collection methods provide multiple opportunities for resolution before relationships become adversarial.

Creating Efficient Complaint Resolution Systems
Despite best prevention efforts, some billing complaints will occur. Having efficient resolution systems in place can turn potentially negative experiences into positive ones. Quick response times are crucial – patients who wait days or weeks for responses to billing questions often become increasingly frustrated.
Establish clear escalation procedures that empower front-line staff to resolve routine issues while providing clear pathways for more complex problems. Staff should know when to involve supervisors, billing managers, or patient advocates. Documentation systems should track complaint resolution to identify trends and ensure consistent handling of similar issues.
Empowering staff to make reasonable adjustments, such as waiving late fees or setting up payment plans, can resolve many complaints quickly and demonstrate good faith efforts to work with patients. Clear guidelines about what adjustments staff can make independently versus those requiring supervisor approval help streamline the resolution process.
Leveraging Technology for Better Patient Experience
Technology solutions can address many common sources of billing complaints. Automated appointment reminders can include information about expected costs and insurance requirements. Pre-visit eligibility verification helps identify potential insurance issues before treatment, allowing time to address problems proactively.
Real-time eligibility checking during registration ensures that insurance information is current and coverage is active. This prevents the common scenario where patients receive unexpected bills weeks later because their insurance was inactive or expired at the time of service.
Electronic communication preferences allow patients to choose how they receive billing information, whether through email, text messages, or traditional mail. Automated payment reminders and online payment options make it easier for patients to stay current with their accounts.
Measuring Success and Continuous Improvement
Effective complaint reduction requires ongoing measurement and improvement efforts. Key metrics might include the number of billing complaints per month, average time to resolution, patient satisfaction scores related to billing experiences, and the percentage of complaints resolved on first contact.
Regular patient surveys can provide insights into billing-related satisfaction and identify areas for improvement. Exit interviews with patients who switch providers can reveal whether billing issues contributed to their decision to leave.
Staff feedback is equally valuable, as front-line employees often have insights into recurring problems and potential solutions. Regular team meetings focused on billing issues can generate ideas for process improvements and help identify training needs.
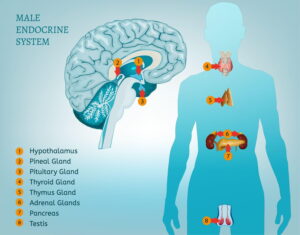
Medical Billing
Medical billing is often confusing. Hospitals and clinics generally bill directly to health insurers or HMOs, and certain billing codes are used to identify certain treatments or types of service. In addition, patients are sometimes asked to pay a portion of a bill through a co-pay or all of a bill if they don’t have health coverage or if the type of service is not covered under their particular health plan.
If you believe a health care provider is mistakenly attempting to collect charges, you may want to consider the following information.
- Keep all of your records. For instance, if you are being double-billed for something, it is important to have all past bills and communication with the provider on hand.
- Contact the provider and ask them about the charges you believe are incorrect.
- • If you tell a medical provider or insurance company that you believe there is a mistake in your medical bill or insurance coverage, the medical provider or insurance company is required by Minnesota law to review the bill. A medical provider cannot begin trying to collect the medical bill until they have finished the review. If they find an error during their review, they are required to fix the error and refund any money you overpaid them within 30 days. If they conclude the bill was correct, they must explain to you in detail why the bill is accurate.
Sometimes a provider may use a collection agency or lawyer to collect bills that are not paid. If you would like to make a complaint about a provider involved in questionable billing practices, you may contact the Attorney General’s Office. The Attorney General’s Office publishes a free brochure called The Credit Handbook that discusses your collection law rights and how to dispute a debt. We also publish a flyer called Medical Billing Pointers. In addition, the Minnesota Department of Commerce regulates and accepts complaints concerning such activity, and can be reached by phone at (651) 539-1500.
Charging the Uninsured a Fairer Price and Changing Collection Practices
Although health plans, employers, and the government are able to negotiate steep discounts for health care charges, many hospitals and other providers have charged the uninsured their “sticker” or “list” prices, which are much higher. Most Minnesota hospitals signed agreements with the Minnesota Attorney General’s Office to offer uninsured patients a fairer price for hospital services and improve the debt collection practices that currently exist in the hospital industry.
The agreements will help those patients who do not have health insurance in the following way:
- The hospital will not charge a patient whose annual household income is less than $125,000 for any uninsured treatment in an amount greater than the amount the provider would be reimbursed for that service or treatment from the insurance company which provided that hospital with the most revenue for its services in the previous calendar year.
The agreements also establish standards that hospitals and certain clinics will follow when attempting to collect medical debt from patients.
- Prior to filing any lawsuit against a patient or referring any patient’s account to a debt collection agency or attorney, the hospitals and clinics will undertake due diligence to ensure that:
- The patient owes the debt,
- All insurance companies that may be responsible to pay the claim have been billed,
- The patient has been offered a payment plan if the patient cannot afford to pay the entire bill at once, and
- The patient has been offered any free or discounted care for which the patient may be eligible under the hospital’s charity care policy.
- Prior to garnishing any patient’s wages or bank account, the hospitals and clinics will undertake the same due diligence to ensure that impoverished patients are not improperly garnished. To ensure adequate judicial supervision over such actions, the hospitals and clinics will not pursue any garnishment without first obtaining a judgment against the patient.
- Hospitals and clinics will adopt a number of other specific debt collection reforms. For instance:
- They will develop a zero tolerance policy for abusive and harassing debt collection conduct;
- They will instruct their attorneys not to petition to have a debtor arrested as a result of a debt collection action;
- They will periodically review their contracts with outside debt collection agencies and attorneys to ensure they are acting in accordance with the law and the hospital’s mission;
- They will ensure that all lawsuits are promptly filed in court, that service of the lawsuit upon the patient is documented, and that no default judgment is obtained against the patient until the patient has been given a fair opportunity to respond.
- Hospitals and clinics will establish a streamlined process for patients to question or dispute bills, including a toll-free number they may call and an address to which they may write. Hospitals and clinics will promptly respond to patient inquiries. Collection notices will list the number for the Minnesota Attorney General’s Office for patients who need assistance.
As of the publication of this brochure, most Minnesota hospitals had signed agreements with the Minnesota Attorney General. If you are unsure about whether your hospital is covered by such an agreement, please contact us.
Conclusion
Reducing patient billing complaints requires a comprehensive approach that addresses communication, processes, technology, and staff capabilities. Success depends on creating transparency throughout the billing cycle, empowering staff to resolve issues effectively, and maintaining focus on the patient experience even during financial interactions.
The investment in complaint reduction pays dividends through improved patient satisfaction, reduced administrative costs, better staff morale, and enhanced organizational reputation. Healthcare providers who prioritize clear communication, efficient processes, and patient-centered billing practices create competitive advantages while fulfilling their mission to serve patients effectively.
Most importantly, reducing billing complaints supports the fundamental healthcare goal of maintaining trust between providers and patients. When financial interactions are handled professionally and transparently, patients can focus on their health and recovery rather than worrying about unexpected bills or navigating confusing billing processes. This creates better outcomes for everyone involved and strengthens the healthcare organization’s ability to serve its community effectively.



