The $2 Billion Problem: Why GI Claims Coding Errors Are Bleeding Healthcare Revenue – And the Complete Roadmap to Stop Them
Coding Errors
Coding Errors
Every day, gastroenterology practices across America are losing thousands of dollars to preventable coding errors. Here’s how to plug the leak.
The numbers are staggering: healthcare providers lose an estimated $2 billion annually due to gastrointestinal (GI) claims coding errors. That’s not a typo – billion with a “B.” Behind every denied claim, every delayed payment, and every frustrated administrator lies a simple truth: GI coding is one of the most complex specialties in medical billing, where a single misplaced modifier or missing documentation detail can cost thousands in lost revenue.
If you’re reading this, chances are you’ve felt the sting of GI claim denials. Maybe you’re a coding manager watching your denial rates climb, a GI practice administrator struggling with cash flow, or a physician wondering why your perfectly performed procedures keep getting rejected by insurance companies. You’re not alone – and more importantly, these problems are entirely solvable.
Why GI Coding Feels Like Navigating a Minefield
Gastroenterology stands apart from other medical specialties in its coding complexity. Unlike straightforward office visits or routine surgeries, GI procedures exist in a gray area where diagnostic intent can shift mid-procedure, where bundling rules seem to change with every payer update, and where the difference between “screening” and “surveillance” can determine whether a patient pays nothing or faces a $1,200 bill.
Consider this real-world scenario: A 55-year-old patient arrives for a routine screening colonoscopy. During the procedure, you discover and remove three polyps from different locations. What started as a simple screening (Z12.11) with modifier 33 suddenly involves multiple CPT codes, specific anatomical modifiers, and a shift from preventive to diagnostic coding. Miss any element of this documentation chain, and your claim joins the 15-20% of GI claims that face denials or delays.
The challenge isn’t just clinical – it’s operational, financial, and increasingly, it’s about survival in an era of razor-thin margins and aggressive payer auditing.
The Financial Reality: What These Errors Actually Cost
Before diving into solutions, let’s quantify the problem. The average GI practice processes 500-1,500 claims monthly. A modest 10% error rate (below the industry average) means 50-150 problematic claims every month. At an average reimbursement of $800 per GI procedure, that’s $40,000-$120,000 in monthly revenue at risk.
But the real cost goes beyond delayed payments:
- Administrative Burden: Each denied claim requires 3-5 hours of staff time for appeals and resubmission
- Cash Flow Disruption: Delayed payments can force practices to carry expensive bridge financing
- Audit Risk: High error rates trigger payer audits that can result in significant clawbacks
- Provider Frustration: Physicians spending time on billing issues instead of patient care
The practices that master GI coding don’t just avoid these costs – they gain a competitive advantage through faster reimbursement, better cash flow, and the ability to focus on patient care rather than claims management.
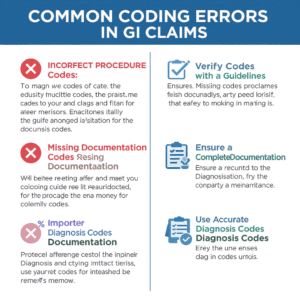
The 8 Critical Error Categories That Drain Revenue
1. The Documentation Deficit: When “Good Enough” Isn’t Good Enough
The Problem: This remains the number one reason for GI claim denials. Medical necessity isn’t just about performing the right procedure – it’s about painting a crystal-clear picture of why that procedure was essential for that specific patient at that specific time.
Real-World Example:
- Weak Documentation: “Patient presents for colonoscopy. Procedure completed without complications.”
- Strong Documentation: “52-year-old patient presents with 6-month history of intermittent rectal bleeding, change in bowel habits (increased frequency, pencil-thin stools), and 15-pound unintentional weight loss. Family history significant for colorectal cancer in father at age 58. Physical exam reveals trace blood on digital rectal examination. Given red flag symptoms and family history, diagnostic colonoscopy indicated to rule out malignancy.”
The Fix:
- Implement SOAP-R Documentation: Subjective complaints, Objective findings, Assessment, Plan, plus Rationale for the specific procedure
- Use the “Would a Peer Agree?” Test: Could another GI physician read your note and immediately understand why this procedure was necessary?
- Create Documentation Checklists: Specific prompts for common procedures that ensure all medical necessity elements are captured
2. The CPT Code Labyrinth: Precision Matters More Than You Think
The Problem: GI procedures often involve similar techniques with subtle but crucial differences. The distinction between an EGD with biopsy (43239) and an EGD with band ligation (43244) might seem minor, but it represents hundreds of dollars in reimbursement difference.
Common Traps:
- Coding diagnostic procedures when therapeutic work was performed
- Missing combination codes that provide higher reimbursement
- Using outdated codes after annual CPT updates
The Fix:
- Master the Decision Trees: Create flowcharts for common procedures that guide coders through the correct code selection process
- Invest in Specialized Training: Generic coding education isn’t enough – GI coding requires specialty-specific expertise
- Establish Physician-Coder Review Sessions: Monthly meetings where physicians can clarify procedure nuances and coders can highlight documentation needs
3. The Modifier Maze: Small Details, Big Impact
Modifiers in GI coding aren’t just administrative footnotes – they’re the difference between proper reimbursement and claim denials. Yet modifier errors plague even experienced coding teams.
High-Risk Scenarios:
- Modifier 59 Overuse: The “distinct procedural service” modifier is often misapplied, leading to unbundling errors
- Screening vs. Diagnostic Confusion: Misusing modifier 33 or PT can shift patient financial responsibility dramatically
- Bilateral Procedure Oversights: Missing modifier 50 on appropriate procedures leaves money on the table
The Strategic Approach:
- Create Modifier Decision Matrices: Visual guides that help coders determine the correct modifier for common scenarios
- Implement Double-Verification: Have a second coder review all claims with modifiers before submission
- Track Modifier-Related Denials: Identify patterns and provide targeted retraining
4. ICD-10-CM Precision: The Diagnostic Story Must Be Complete
The transition to ICD-10-CM brought unprecedented specificity requirements, but many practices still code as if ICD-9 rules apply. This “good enough” approach costs practices thousands in denied claims.
Specificity Requirements:
- Anatomical Location: “Polyp of colon” isn’t sufficient – specify ascending, transverse, descending, or sigmoid
- Severity and Type: “Gastritis” versus “chronic atrophic gastritis with dysplasia” are entirely different reimbursement scenarios
- Episode of Care: Initial encounter, subsequent encounter, or sequela can affect payment
Mastery Strategies:
- Develop ICD-10-CM Quick Reference Guides: Specialty-specific guides that highlight the most commonly needed codes and their specificity requirements
- Use Clinical Decision Support Tools: Software that prompts for the additional specificity required for complete coding
- Regular Physician Education: Help providers understand that their diagnostic language directly impacts coding accuracy
5. The Bundling Trap: When More Isn’t Better
National Correct Coding Initiative (NCCI) edits exist to prevent inappropriate unbundling, but the rules can be counterintuitive. Many practices inadvertently leave money on the table by under-coding, while others trigger audits through inappropriate unbundling.
Common Bundling Errors:
- Billing diagnostic and therapeutic procedures separately when they’re part of the same encounter
- Missing opportunities to use combination codes that provide higher reimbursement
- Incorrectly applying modifier 59 to “break” edits that shouldn’t be broken
Best Practices:
- Monthly NCCI Edit Reviews: Stay current with quarterly updates and understand how they apply to your common procedures
- Invest in Advanced Coding Software: Tools that automatically apply edits and flag potential bundling issues
- Create Internal Bundling Guidelines: Written policies for your most common procedures that specify exactly when unbundling is appropriate
6. The Screening-Diagnostic Dilemma: Navigation Through Policy Complexity
Perhaps no area of GI coding causes more confusion than the distinction between screening and diagnostic procedures, especially when a screening procedure discovers abnormalities requiring intervention.
The Challenge: A routine screening colonoscopy that discovers and removes polyps transforms from a preventive service (often with zero patient cost-sharing) to a diagnostic/therapeutic procedure (with standard deductibles and copays applying).
Payer-Specific Variations:
- Medicare: Uses modifier PT to indicate a screening that became diagnostic
- Commercial Payers: Vary widely in their handling of screening-to-diagnostic transitions
- ACA Preventive Services: Have specific rules about when screening benefits are preserved
Navigation Strategy:
- Create Payer-Specific Flowcharts: Visual guides showing how each major payer handles screening-to-diagnostic transitions
- Implement Pre-Procedure Verification: Confirm screening benefits and understand how they change if abnormalities are found
- Patient Communication Protocols: Inform patients about potential cost implications if screening procedures become therapeutic
7. Location, Location, Location: The Anatomy of Accurate Coding
Vague anatomical references in operative reports create a cascade of coding problems. “Polyp removed from colon” provides insufficient information for accurate coding, reimbursement optimization, and medical necessity support.
Required Specificity:
- Exact Anatomical Location: Cecum, ascending colon, hepatic flexure, transverse colon, splenic flexure, descending colon, sigmoid colon, or rectum
- Size and Characteristics: Small (< 1cm), large (> 2cm), pedunculated, sessile, flat
- Removal Method: Cold forceps, hot forceps, snare, EMR (endoscopic mucosal resection), ESD (endoscopic submucosal dissection)
Documentation Enhancement:
- Structured Templates: Electronic health record templates that prompt for specific anatomical and procedural details
- Visual Documentation: Digital photos or drawings that clearly show lesion locations
- Standardized Terminology: Consistent use of anatomical terms across all providers
8. Anesthesia Integration: The Often-Overlooked Revenue Stream
GI procedures increasingly require anesthesia services, creating additional coding complexity and revenue opportunities that many practices inadequately capture.
Common Oversights:
- Incorrect Anesthesia CPT Codes: Using base units that don’t match the actual procedure performed
- Time Unit Miscalculations: Errors in converting actual anesthesia time to billable time units
- Missing ASA Modifiers: Physical status modifiers that can significantly impact reimbursement
- Poor Communication: Inadequate information sharing between GI and anesthesia billing teams
Optimization Strategies:
- Dedicated Anesthesia Coding Expertise: Either in-house specialists or reliable outsourcing partners
- Integrated Documentation Systems: Electronic systems that capture both procedure and anesthesia details in coordinated fashion
- Regular Cross-Training: Ensure GI coders understand anesthesia basics and anesthesia billers understand GI procedures
The Revenue Recovery Roadmap: Implementation Strategies That Work
Phase 1: Assessment and Baseline (Months 1-2)
Comprehensive Claims Analysis:
- Review 6 months of GI claims data to identify denial patterns
- Calculate current error rates by procedure type and payer
- Quantify revenue at risk and administrative costs of current errors
Team Skill Assessment:
- Evaluate current coding team capabilities
- Identify knowledge gaps in GI-specific coding
- Assess physician documentation quality and completeness
Technology Audit:
- Review current coding software capabilities
- Assess integration between clinical documentation and billing systems
- Identify opportunities for automation and error reduction
Phase 2: Foundation Building (Months 3-6)
Education and Training Implementation:
- Enroll coding team in specialized GI coding certification programs
- Implement monthly physician-coder education sessions
- Create specialty-specific coding reference materials and quick guides
Process Standardization:
- Develop written policies for common GI coding scenarios
- Implement pre-procedure verification protocols
- Establish physician query processes for incomplete documentation
Technology Enhancement:
- Upgrade to advanced coding software with GI-specific edit checks
- Implement clinical documentation improvement tools
- Establish automated claim scrubbing processes
Phase 3: Advanced Optimization (Months 7-12)
Performance Monitoring:
- Implement real-time denial tracking and analysis
- Establish monthly performance dashboards
- Create accountability measures for both coding and clinical teams
Continuous Improvement:
- Conduct quarterly coding audits with detailed feedback
- Establish appeals management expertise and processes
- Implement predictive analytics to identify high-risk claims before submission
Revenue Optimization:
- Analyze reimbursement patterns to identify undercoding opportunities
- Negotiate payer contracts based on improved coding accuracy
- Establish charge capture systems that ensure all services are billed
Phase 4: Mastery and Leadership (Year 2 and Beyond)
Industry Leadership:
- Share best practices through professional organizations
- Participate in coding guideline development and feedback processes
- Establish your practice as a resource for GI coding excellence
Strategic Expansion:
- Use coding mastery as a competitive advantage in provider recruitment
- Leverage improved cash flow for practice expansion and technology investment
- Consider offering coding consulting services to other GI practices
Technology Solutions: The Modern GI Coding Stack
The right technology stack can eliminate many common coding errors while improving efficiency and accuracy. Here’s what leading GI practices use:
Core Coding Software:
- Advanced Edit Checks: Software that automatically applies NCCI edits and payer-specific rules
- Real-Time Claim Scrubbing: Systems that identify potential errors before claim submission
- Integrated Documentation: Tools that link clinical notes directly to coding decisions
Specialized GI Tools:
- Procedure-Specific Templates: Electronic health record templates designed for GI procedures
- Visual Documentation Systems: Digital imaging and diagramming tools for lesion location
- Automated Code Suggestions: AI-powered tools that suggest codes based on documentation
Analytics and Reporting:
- Denial Management Dashboards: Real-time tracking of claim status and denial reasons
- Performance Metrics: KPI tracking for coding accuracy, clean claim rates, and revenue cycle performance
- Predictive Analytics: Tools that identify high-risk claims and potential audit triggers
Measuring Success: KPIs That Matter
Successful GI coding optimization requires consistent measurement and monitoring. Track these critical metrics:
Financial Metrics:
- Clean Claim Rate: Target >95% for GI claims
- Days in A/R: Industry benchmark is <45 days for GI practices
- Net Collection Rate: Should exceed 98% for most GI procedures
- Denial Rate: Target <5% for routine GI procedures
Operational Metrics:
- Time to Submission: Claims should be submitted within 3-5 days of service
- Appeal Success Rate: Should exceed 75% for appealed claims
- Coding Productivity: Benchmark coding rates per FTE for different procedure types
Quality Metrics:
- Audit Results: Regular internal audits should show >95% accuracy
- Payer Audit Outcomes: Track results of external audits and implement corrective actions
- Physician Satisfaction: Survey providers regularly on billing and coding support
The ROI of Getting It Right
Let’s quantify the return on investment for comprehensive GI coding optimization:
Sample Practice Profile:
- 1,000 GI procedures monthly
- Average reimbursement: $800 per procedure
- Current denial rate: 12%
- Target denial rate: 4%
Monthly Impact of Optimization:
- Error Reduction: 80 fewer denied claims monthly
- Direct Revenue Recovery: $64,000 monthly ($768,000 annually)
- Administrative Savings: 240 hours of staff time monthly
- Cash Flow Improvement: Faster collections and reduced carrying costs
Investment Requirements:
- Training and Education: $25,000-50,000 initial investment
- Technology Upgrades: $15,000-30,000 for software and tools
- Process Implementation: $10,000-20,000 in consulting and setup costs
Net ROI: Most practices see 300-500% ROI within the first year of comprehensive GI coding optimization.
Building Your Action Plan: What to Do Monday Morning
Ready to transform your GI coding performance? Here’s your immediate action plan:
Week 1: Data Gathering
- Pull 90 days of GI claims data and denial reports
- Calculate your current error rates by procedure type
- Identify your top 3 denial reasons
Week 2: Team Assessment
- Evaluate current coding team GI expertise
- Survey physicians on documentation challenges
- Review current technology capabilities
Week 3: Quick Wins
- Implement pre-procedure verification for all GI procedures
- Create documentation checklists for your top 5 procedures
- Establish physician query protocols for incomplete notes
Week 4: Strategic Planning
- Develop 90-day improvement plan with specific targets
- Budget for necessary training and technology investments
- Establish baseline metrics and monitoring processes
The Future of GI Coding: Staying Ahead of the Curve
The world of medical coding continues to evolve rapidly. Successful GI practices must anticipate and prepare for upcoming changes:
Emerging Trends:
- AI-Powered Coding: Machine learning tools that can suggest codes based on clinical documentation
- Value-Based Reimbursement: Shift from volume to value will impact GI coding requirements
- Patient Price Transparency: New regulations requiring upfront cost estimates will increase accuracy demands
Preparation Strategies:
- Continuous Education: Establish ongoing training programs that keep pace with industry changes
- Technology Investment: Plan for regular upgrades and new tool adoption
- Industry Participation: Engage with professional organizations and coding committees to influence future standards
Conclusion: Your Revenue Is Waiting
Every day you delay optimizing your GI coding processes, revenue walks out the door. The practices that master these challenges don’t just survive – they thrive, with better cash flow, lower administrative costs, and the financial freedom to focus on what matters most: providing exceptional patient care.
The roadmap is clear, the tools are available, and the ROI is proven. The only question remaining is: when will you start your journey from coding chaos to revenue mastery?
Your patients deserve the best clinical care. Your practice deserves the best coding performance. The time to act is now.
Ready to transform your GI coding performance? Contact our healthcare revenue cycle experts for a complimentary practice assessment and discover how much revenue you could recover in the next 90 days.



