Top Dermatology Coding Errors & How to Fix Them for Maximum Reimbursement
Coding
Coding
Dermatology practices face unique billing challenges that can significantly impact revenue streams. With over 3,000 skin conditions requiring precise documentation and coding, dermatologists must navigate complex CPT codes, evolving payer policies, and intricate procedural distinctions. Industry studies indicate that dermatology practices lose an average of 15-20% of potential revenue due to coding errors, making accuracy not just important—but financially critical.
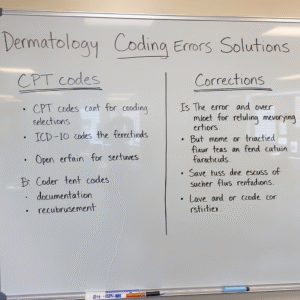
This comprehensive guide examines the most frequent dermatology coding pitfalls and provides actionable solutions to optimize your practice’s reimbursement rates while maintaining compliance with current regulations.
1. Misclassifying Excisions vs. Biopsies vs. Shave Removals
The distinction between these three fundamental dermatological procedures represents one of the most costly coding errors in the specialty. Each procedure type has specific CPT codes, reimbursement rates, and documentation requirements that, when confused, can result in significant revenue loss.
The Error in Detail
The confusion typically stems from misunderstanding the primary intent and technique used during tissue removal. Common mistakes include:
- Billing a shave removal as an excision: This occurs when providers remove a lesion using a tangential or “scooping” technique that doesn’t extend into subcutaneous fat but bill it as a full-thickness excision (11400-11471 series).
- Coding biopsies as excisions: Even when a small lesion is entirely removed during a diagnostic biopsy, it should still be coded as a biopsy (11102-11107 series) if the primary intent was diagnostic rather than therapeutic.
- Excision overcoding: Billing for malignant excision codes (11600-11646) when the final pathology reveals benign tissue, without proper documentation supporting the clinical suspicion of malignancy.
The Comprehensive Fix
Documentation Excellence:
- Record the specific technique used (punch, shave, scalpel excision, electrodesiccation)
- Document the depth of tissue removal (epidermis, dermis, subcutaneous fat)
- Clearly state the primary intent (diagnostic vs. therapeutic)
- Measure and record lesion dimensions before and after removal
- Include clinical rationale for the chosen technique
Education and Training:
- Implement monthly coding refreshers focusing on procedural distinctions
- Create visual aids showing cross-sections of different removal techniques
- Establish clear protocols for when to use each procedure type
- Develop decision trees to guide appropriate code selection
Quality Assurance:
- Institute pre-billing reviews for all tissue removal procedures
- Cross-reference pathology reports with initial coding decisions
- Track patterns in code selections to identify potential training needs
2. Incorrect Use of Modifiers 25 and 59
Modifiers serve as critical communication tools between providers and payers, but their misuse can trigger immediate denials, payment delays, and increased audit risk. Dermatology practices are particularly scrutinized for modifier usage due to the frequent combination of evaluation and management services with procedures.
The Error Expanded
Modifier 25 Complications:
- Appending Modifier 25 when the E/M service is merely pre-procedural work
- Using the modifier for routine post-procedure checks
- Failing to document the separate and distinct nature of the E/M service
- Applying Modifier 25 to E/M services that don’t meet the “above and beyond” threshold
Modifier 59 Misapplication:
- Attempting to unbundle procedures that are inherently part of a comprehensive service
- Using Modifier 59 instead of more specific modifiers (XE, XP, XS, XU) when available
- Applying the modifier without clear anatomical or temporal separation
Enhanced Solutions
Payer-Specific Guidelines:
- Research and document each major payer’s specific modifier policies
- Create payer-specific coding guides for staff reference
- Establish relationships with payer representatives for clarification on complex cases
Documentation Standards:
- For Modifier 25: Document the separate problem addressed during the E/M service
- Include time stamps when procedures and E/M services occur at different times
- Clearly differentiate between pre-procedural assessment and comprehensive evaluation
Technology Integration:
- Implement EHR alerts that prompt for modifier justification
- Use coding software that flags potential modifier misuse
- Develop automated reports tracking modifier usage patterns

3. Inaccurate Lesion Coding: Size, Location, and Pathology Alignment
Dermatology’s diverse pathology requires precise coding that reflects lesion characteristics, anatomical locations, and final diagnostic outcomes. Errors in this area can result in both under-reimbursement and compliance violations.
Detailed Error Analysis
Size-Related Errors:
- Failing to include excision margins in size calculations
- Inconsistent measurement techniques across providers
- Not accounting for tissue contraction during measurement
Location-Specific Mistakes:
- Misclassifying anatomical sites (e.g., trunk vs. scalp/neck/hands/feet)
- Using incorrect codes for complex anatomical areas
- Failing to recognize premium payment areas
Pathology Misalignment:
- Billing malignant codes when pathology reveals benign lesions
- Not adjusting codes when pathology contradicts clinical assessment
- Delays in coding corrections after pathology results
Comprehensive Correction Strategy
Standardized Measurement Protocols:
- Train all staff on consistent measurement techniques
- Use standardized measuring tools across all exam rooms
- Document measurements before and after local anesthesia injection
- Include photographic documentation when appropriate
Anatomical Coding Expertise:
- Create anatomical reference charts for each exam room
- Develop location-specific coding quick reference guides
- Regularly review anatomical boundaries with coding staff
Pathology Integration Systems:
- Establish protocols for reviewing pathology reports within 24-48 hours
- Create systems for coding corrections based on final pathology
- Track accuracy rates for initial clinical assessments vs. final pathology
4. Documentation Deficiencies: The Foundation of Successful Billing
Documentation serves as the foundation for all medical billing, but dermatology’s visual nature and procedural complexity demand particularly detailed record-keeping. Inadequate documentation remains the leading cause of claim denials and audit failures.
Common Documentation Failures
- Vague procedural descriptions lacking specific techniques
- Missing medical necessity justifications
- Incomplete lesion characterizations
- Absent risk factor documentation
- Insufficient post-procedure care instructions
Advanced Documentation Solutions
Template Optimization:
- Design procedure-specific templates that capture all required elements
- Include mandatory fields for critical information
- Create drop-down menus for common descriptions
- Implement auto-population features for frequently used phrases
Photography Integration:
- Establish protocols for clinical photography
- Use images to support medical necessity documentation
- Create standardized photo series for before/after comparisons
- Ensure HIPAA compliance in image storage and transmission
Voice Recognition Enhancement:
- Implement advanced voice recognition software
- Create custom vocabularies for dermatology terminology
- Train providers on efficient dictation techniques
- Establish quality review processes for voice-generated notes

5. Advanced Denial Management and Revenue Recovery
Effective denial management extends beyond simple resubmission—it requires systematic analysis, proactive prevention, and strategic appeal processes that can recover significant lost revenue.
Sophisticated Denial Analysis
Pattern Recognition:
- Implement analytics software to identify denial trends
- Track denial rates by provider, payer, and procedure type
- Analyze seasonal variations in denial patterns
- Monitor changes following payer policy updates
Root Cause Investigation:
- Categorize denials by type (coding, coverage, authorization, etc.)
- Assign specific staff members to investigate different denial categories
- Create action plans for each common denial reason
- Establish timelines for denial resolution
Strategic Appeal Processes
Multi-Level Appeal Strategy:
- Develop standardized appeal letter templates
- Create escalation procedures for complex denials
- Establish relationships with payer medical directors
- Implement peer-to-peer review processes when appropriate
Revenue Recovery Optimization:
- Calculate the financial impact of different denial types
- Prioritize high-value appeals over low-value claims
- Track appeal success rates by payer and issue type
- Analyze cost-benefit ratios for appeal investments
6. Technology Integration and Future-Proofing
Modern dermatology practices must leverage technology to maintain coding accuracy and optimize reimbursement in an increasingly complex regulatory environment.
Advanced Technology Solutions
Artificial Intelligence Integration:
- Implement AI-powered coding assistance tools
- Use machine learning algorithms to identify coding patterns
- Deploy automated claim scrubbing technology
- Utilize predictive analytics for denial prevention
Real-Time Eligibility Verification:
- Integrate real-time insurance verification systems
- Implement automated prior authorization workflows
- Create patient portal functionality for insurance updates
- Establish automated eligibility checking protocols
Regulatory Compliance and Updates
Staying Current:
- Subscribe to multiple coding update services
- Participate in dermatology-specific coding webinars
- Maintain relationships with coding consultants
- Implement systematic review processes for code changes
Audit Preparedness:
- Conduct regular internal audits using external audit criteria
- Maintain comprehensive documentation retention systems
- Create audit response protocols and documentation
- Establish relationships with healthcare attorneys when needed

Conclusion: Building a Robust Revenue Cycle
Maximizing dermatology reimbursement requires a comprehensive approach that combines technical expertise, systematic processes, and ongoing education. By addressing these common coding errors through structured improvements in documentation, staff training, technology integration, and denial management, practices can typically recover 10-15% of lost revenue within the first year of implementation.
The key to success lies not in perfection, but in systematic improvement and proactive management of the revenue cycle. Regular assessment, continuous education, and adaptive strategies will ensure your dermatology practice maintains optimal financial health while providing excellent patient care.
Success in dermatology billing is measured not just by claim acceptance rates, but by the practice’s ability to capture appropriate reimbursement for the complex, specialized care dermatologists provide. Through careful attention to these coding fundamentals and implementation of best practices, your practice can achieve both financial success and regulatory compliance in today’s challenging healthcare environment.



