7 Critical Dermatology Coding Pitfalls: Safeguard Your Revenue
Dermatology Coding
Dermatology Coding
In the complex landscape of medical billing, dermatology practices face unique challenges that can significantly impact their revenue streams. With constantly evolving coding requirements, insurance regulations, and documentation standards, even the most experienced billing teams can fall into costly traps. Understanding and avoiding these critical coding pitfalls isn’t just about compliance—it’s about protecting your practice’s financial health and ensuring you receive appropriate compensation for the specialized care you provide.
The stakes are higher than ever. Incorrect coding can lead to claim denials, audit triggers, compliance issues, and substantial revenue loss. For dermatology practices, where procedures range from routine skin examinations to complex surgical interventions, precise coding becomes paramount. Let’s explore the seven most critical coding pitfalls that dermatology practices encounter and learn how to safeguard your revenue against these common mistakes.
1. Misunderstanding the Global Surgical Package
One of the most costly mistakes in dermatology coding involves misunderstanding what’s included in the global surgical package. The global period concept encompasses the pre-operative, intra-operative, and post-operative services related to a surgical procedure, and many practices inadvertently leave money on the table or risk overcoding violations.
The global surgical package typically includes the initial consultation or evaluation when it leads directly to the decision for surgery, the surgical procedure itself, and all routine post-operative care within the designated global period. For minor procedures with a 10-day global period, this includes normal post-operative visits, while major procedures with a 90-day global period encompass more extensive follow-up care.
Common errors include billing separately for routine post-operative visits that fall within the global period, failing to bill for complications or unrelated services that occur during the global period, and not understanding when modifier -24 (unrelated evaluation and management service during a postoperative period) should be applied. Additionally, practices often struggle with distinguishing between routine healing and complications that warrant separate billing.
To avoid these pitfalls, establish clear protocols for documenting and coding services during global periods. Train your staff to recognize when complications arise that justify separate billing, and ensure proper use of modifiers when providing unrelated services during the global period. Maintain detailed documentation that clearly supports any services billed separately from the global package.
2. Incorrect Application of Evaluation and Management (E/M) Codes
Evaluation and Management coding represents a significant portion of dermatology revenue, yet it’s frequently miscoded, leading to both undercoding and overcoding scenarios. The complexity of dermatology E/M services, particularly when combined with procedures, creates numerous opportunities for error.
Many practices struggle with determining the appropriate level of E/M service, especially when the visit includes both evaluation of skin conditions and procedural work. The key lies in understanding that the E/M service must be significant and separately identifiable from the procedure to warrant separate billing. Simply examining the area before a procedure doesn’t typically justify a separate E/M code.
Documentation requirements for E/M services in dermatology must support the level of service billed. This includes appropriate history taking, examination details specific to dermatologic conditions, and medical decision-making that reflects the complexity of the patient’s condition. Under the current guidelines, practices must ensure their documentation supports the time spent or the level of medical decision-making claimed.

Common mistakes include routinely billing the same level E/M code regardless of service complexity, failing to document sufficient detail to support higher-level codes, billing separate E/M services for brief assessments that are integral to procedures, and not understanding when modifier -25 is appropriately applied to indicate a significant, separately identifiable E/M service.
Implement regular chart audits focusing on E/M documentation and coding accuracy. Provide ongoing education to providers about documentation requirements and ensure coding staff understand the nuances of when E/M services can be billed separately from procedures.
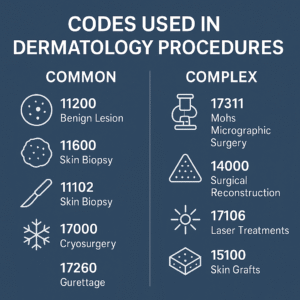
3. Destruction Procedure Coding Errors
Destruction procedures, including treatment of benign and malignant lesions, represent a significant portion of dermatology services and are frequently miscoded. These errors can result in substantial revenue loss or compliance issues, making accurate coding crucial for practice success.
The most common error involves confusion between destruction of benign versus malignant lesions. CPT codes 17000-17004 are specifically for destruction of benign lesions, while codes 17260-17286 are for destruction of malignant lesions. Using the wrong code series can result in significant reimbursement differences and potential audit red flags.
Another frequent mistake involves counting lesions incorrectly. For benign lesion destruction, the first lesion is coded with 17000, and lesions 2-14 are coded with 17003 for each additional lesion. Many practices incorrectly code multiple units of 17000 or fail to understand the unit limitations for these codes.
Size and location requirements add another layer of complexity. Some destruction codes have specific size requirements or anatomical location restrictions that must be carefully observed. Failing to meet these criteria can result in claim denials or downcoding.
Method-specific coding requirements also create confusion. Different destruction methods (cryotherapy, electrosurgery, laser, etc.) may have specific coding requirements or limitations that practices must understand to code accurately.
To prevent these errors, create clear protocols for measuring and documenting lesions before destruction. Ensure your coding staff understands the differences between benign and malignant lesion codes, and implement checks to verify lesion counts and measurements are accurately reflected in coding.
4. Pathology and Laboratory Coding Complications
Dermatology practices frequently perform or order pathology services, creating opportunities for coding errors that can impact revenue and compliance. The complexity of pathology coding, combined with changing regulations around laboratory billing, makes this area particularly challenging.
Professional versus technical component billing represents a major source of confusion. When billing for pathology services, practices must understand whether they’re billing for the professional component (interpretation), technical component (specimen processing), or global service (both components). Incorrect modifier usage (-26 for professional component, -TC for technical component) can result in improper reimbursement.
In-office versus reference laboratory considerations add another layer of complexity. Different rules apply when pathology services are performed in-office versus sent to reference laboratories, and practices must understand their billing responsibilities in each scenario.

Specimen adequacy and rebiopsy situations create coding challenges when initial specimens are inadequate or when multiple specimens are taken from the same site. Understanding how to code these scenarios appropriately is crucial for accurate reimbursement.
Multiple specimen billing requires careful attention to whether specimens are from the same or different anatomical sites, as this affects coding and reimbursement. Each unique site typically warrants separate coding, but specimens from the same site may be subject to bundling rules.
Establish clear protocols for pathology specimen handling and coding. Ensure your team understands the difference between professional and technical components, and maintain accurate documentation of specimen sources and adequacy.
5. Modifier Misuse and Omission
Modifiers play a crucial role in dermatology coding, providing additional information about services performed and ensuring appropriate reimbursement. However, modifier misuse or omission represents one of the most common coding errors, often resulting in claim denials or incorrect payment amounts.
Modifier -25 is perhaps the most important and misused modifier in dermatology. It indicates that a significant, separately identifiable evaluation and management service was performed on the same day as a procedural service. Many practices either overuse this modifier for routine pre-procedure assessments or fail to use it when truly warranted.
Anatomical modifiers (-LT, -RT, -E1 through -E4, -F1 through -F9, -T1 through -T9, etc.) are essential for indicating specific body locations, particularly important for bilateral procedures or multiple procedures on different digits or anatomical areas. Omitting these modifiers can result in claim denials or incorrect bundling.
Modifier -59 and its more specific counterparts (-XE, -XP, -XS, -XU) are used to indicate distinct procedural services. In dermatology, where multiple procedures are often performed in the same session, proper use of these modifiers is crucial for avoiding inappropriate bundling and ensuring full reimbursement.
The -76 (repeat procedure by same physician) and -77 (repeat procedure by another physician) modifiers are important when procedures must be repeated, while -78 (unplanned return to operating room) may apply in specific surgical scenarios.
Create modifier checklists for common scenarios and provide regular training on proper modifier usage. Implement system checks to ensure appropriate modifiers are applied consistently and accurately.
6. Bundling and Unbundling Issues
Understanding which procedures can be billed together and which are subject to bundling rules is crucial for dermatology practices. The National Correct Coding Initiative (NCCI) edits and Medicare’s bundling policies significantly impact reimbursement and require careful attention to avoid compliance issues.
Many dermatology procedures are subject to bundling when performed during the same session or in the same anatomical area. For example, certain biopsy and excision combinations may be bundled, requiring specific modifiers to bill separately when appropriate.
Column 1/Column 2 edits represent the most common bundling scenario, where one procedure (Column 2) is considered integral to another procedure (Column 1) and typically cannot be billed separately. However, appropriate modifiers may override these edits when procedures are distinct and separately identifiable.
Same-session procedure combinations require careful consideration of bundling rules. Multiple procedures performed during the same visit may be subject to multiple procedure payment reductions or complete bundling, depending on the specific procedures and anatomical locations involved.
Site-specific bundling rules add complexity when multiple procedures are performed on the same anatomical area. Understanding when procedures are considered part of the same anatomical site versus separate sites is crucial for accurate coding.
Stay current with NCCI edits and bundling policies through regular updates and training. Implement coding software that includes current bundling logic and provides alerts for potential bundling issues.
7. Documentation Deficiencies
Perhaps the most fundamental pitfall affecting dermatology coding is inadequate documentation. Without proper documentation, even correctly assigned codes can be challenged, leading to claim denials, audit findings, and revenue loss.
Clinical documentation must support the level of service billed and provide sufficient detail for code assignment. This includes detailed descriptions of lesions, anatomical locations, sizes, characteristics, and treatment rationale. Generic or template-driven documentation often fails to provide the specificity required for accurate coding.
Procedure documentation requirements extend beyond basic procedure notes to include specific details required for various code assignments. Size measurements, anatomical locations, depths of procedures, and closure methods all impact code selection and must be thoroughly documented.
Medical necessity documentation is crucial for supporting services provided, particularly for cosmetic versus medical procedures. Clear documentation of medical indications helps prevent claim denials and supports the medical necessity of services billed.
Time-based documentation becomes important when billing based on time spent, particularly for certain E/M services or prolonged service codes. Accurate time documentation must reflect face-to-face time with patients and support the services billed.
Implement documentation templates that prompt for required elements while allowing for individualized patient care notes. Provide regular training on documentation requirements and conduct periodic audits to identify and address documentation deficiencies.
Protecting Your Practice’s Revenue
Avoiding these critical coding pitfalls requires a comprehensive approach that combines education, systems, and ongoing monitoring. Regular staff training, current coding resources, and systematic audit processes help identify and prevent coding errors before they impact revenue.
Invest in quality coding education and resources, including professional development for coding staff and regular updates on coding changes. Implement robust quality assurance processes that include pre-billing chart reviews and post-payment audits to identify trends and opportunities for improvement.
Consider engaging qualified coding consultants or auditors to provide objective assessments of your coding accuracy and identify areas for improvement. Many practices find that professional coding assessments quickly pay for themselves through improved accuracy and revenue optimization.
Finally, maintain open communication between clinical and administrative staff to ensure coding accurately reflects the services provided. Regular meetings between providers and coding staff help identify and resolve coding challenges before they become systematic problems.
By understanding and actively avoiding these seven critical coding pitfalls, dermatology practices can protect their revenue, maintain compliance, and focus on what matters most—providing excellent patient care. The investment in proper coding practices pays dividends through improved cash flow, reduced denials, and decreased audit risk, ultimately supporting the long-term success of your practice.