7 Critical Dermatology Coding Errors: Safeguard Your Revenue!
Dermatology Coding Errors
Dermatology Coding Errors
Dermatology practices face unique challenges in medical coding that can significantly impact their financial health. With the specialty encompassing everything from routine skin screenings to complex Mohs surgeries, the coding landscape is intricate and constantly evolving. Revenue cycle management in dermatology requires precision, attention to detail, and a deep understanding of both clinical procedures and coding guidelines.
The financial stakes are high. According to industry data, coding errors can result in claim denial rates of up to 15% in dermatology practices, translating to substantial revenue losses. Beyond immediate payment delays, these errors can trigger costly audits, compliance issues, and even legal complications. For a typical dermatology practice, this could mean losing hundreds of thousands of dollars annually due to preventable coding mistakes.
To help you protect your practice’s financial stability and ensure optimal reimbursement, we’ve identified seven critical dermatology coding errors that demand your immediate attention. Understanding and avoiding these pitfalls will not only improve your cash flow but also enhance your practice’s overall operational efficiency.
1. Inadequate and Non-Specific Documentation
The Error: Poor documentation is the foundation of most coding problems in dermatology. When medical records fail to tell the complete, legible story of a patient encounter, coders are left to make assumptions that often lead to incorrect code selection. This is particularly problematic in dermatology, where visual findings, lesion characteristics, and procedural details are crucial for accurate coding.
Common documentation deficiencies include vague descriptions of lesions, missing anatomical locations, incomplete procedure notes, and failure to document medical necessity. For example, describing a lesion simply as “suspicious” without detailing size, color, texture, or specific characteristics makes it impossible to select appropriate diagnostic codes.
The Solution: Implement a comprehensive documentation strategy that follows the principle “if it’s not documented, it didn’t happen.” Every clinical note should be complete, legible, specific, and support every service and diagnostic code submitted.
Develop standardized templates for common procedures that include essential elements such as:
- Detailed lesion descriptions (size, color, location, morphology, symptoms)
- Clear procedural notes with technique, instruments used, and complications
- Medical necessity justification for each service
- Patient response and follow-up plans
- Precise anatomical locations using standardized terminology
Train your clinical staff to use specific medical terminology and avoid ambiguous abbreviations. Consider implementing voice recognition software or structured data entry systems to ensure consistency and completeness. Regular documentation audits can help identify and correct recurring deficiencies before they impact revenue.

2. Incorrect Use of Modifiers
The Error: Modifiers provide crucial additional information about services or procedures, and their misuse is a frequent source of claim denials in dermatology. Common modifier errors include failing to append necessary modifiers for multiple lesion removals, incorrect application of bilateral procedure modifiers, or inappropriate use of the -59 modifier for services that don’t meet the “distinct procedural service” criteria.
For instance, when performing multiple biopsies during a single session, failure to use appropriate modifiers can result in payment for only one procedure, significantly reducing reimbursement. Similarly, confusion about when to use -25 modifiers for evaluation and management services can lead to bundling issues.
The Solution: Develop comprehensive modifier training for your coding team, focusing on dermatology-specific applications. Key modifiers to master include:
- Modifier -25: Significant, separately identifiable E/M service on the same day as a procedure
- Modifier -59: Distinct procedural service (use cautiously and only when documentation supports truly separate services)
- Modifier -51: Multiple procedures (often applied automatically by payers)
- Modifier -50: Bilateral procedure
- Modifier -RT/LT: Right and left side designations
- Modifier -XS, -XE, -XP, -XU: More specific alternatives to -59 where appropriate
Create coding guidelines and decision trees to help staff determine appropriate modifier usage. Regular coding audits should specifically review modifier application to ensure compliance and optimal reimbursement. Remember that modifier -59 is heavily audited, so use it only when documentation clearly supports a separate and distinct service.
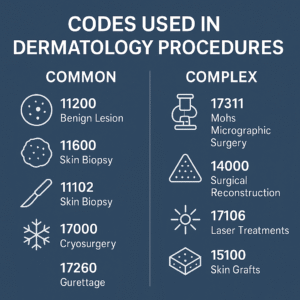
3. Confusion Between Excision and Destruction Codes
The Error: Dermatology frequently involves lesion removal, but the distinction between excision (surgical cutting and removal) and destruction (removal through methods like cryotherapy, electrosurgery, or laser) is fundamental for accurate coding. Misclassifying these procedures is one of the most common and costly errors in dermatology coding.
The confusion often stems from inadequate documentation of the actual technique used or misunderstanding of the clinical differences between these approaches. Using an excision code for a destruction procedure, or vice versa, can result in claim denials or inappropriate reimbursement levels.
The Solution: Ensure clear understanding of the clinical and coding differences between excision and destruction procedures:
Excision procedures:
- Involve full-thickness removal of tissue using a scalpel or similar instrument
- Typically require closure (sutures, skin grafts, or flaps)
- Include margin documentation
- Often send specimens for pathological examination
- Use CPT codes 11400-11646 series
Destruction procedures:
- Remove lesions through ablative methods (cryotherapy, electrocautery, laser, chemical)
- Don’t typically require closure
- May or may not generate tissue for pathology
- Use CPT codes 17000-17999 series
Implement procedure-specific documentation templates that clearly capture the technique used, instruments employed, and closure method. Train clinical staff to use precise terminology in operative notes that clearly distinguishes between these approaches. Consider using standardized procedure templates that automatically prompt for appropriate documentation elements.
4. Failing to Bill for Multiple Procedures or Appropriate Complexity Levels
The Error: Many dermatology practices inadvertently leave money on the table by failing to identify and bill for all eligible services performed during a single encounter. This includes multiple biopsies, additional lesion removals, or failing to bill appropriate evaluation and management (E/M) levels due to insufficient documentation of complexity.
Another common oversight is not recognizing when separate procedures performed during the same session warrant individual billing. For example, performing both a biopsy and an unrelated cryotherapy treatment should typically be billed separately with appropriate modifiers.
The Solution: Implement systematic charge capture processes that ensure all eligible services are identified and billed appropriately:
For multiple procedures:
- Carefully review each encounter to identify all separately billable services
- Ensure documentation supports each individual procedure
- Apply appropriate modifiers for multiple procedures
- Verify that combination coding rules are followed correctly
For E/M services:
- Use the 2021 E/M guidelines that emphasize medical decision-making complexity
- Document the complexity of problems addressed, data reviewed, and risk assessment
- Ensure that E/M services are separately identifiable from procedural services when billing with -25 modifier
- Train providers on documentation requirements for different E/M levels
Develop charge capture tools and checklists that help identify all potential billable services during each encounter. Consider implementing real-time coding assistance software that can flag potential missed charges or coding opportunities.
5. Errors with Biopsy and Lesion Removal Code Selection
The Error: Confusion between biopsy codes (11102-11107) and lesion excision codes (11400-11646) is common and costly. The distinction lies in the intent and extent of the procedure: biopsies are diagnostic sampling procedures, while excisions involve complete lesion removal with therapeutic intent.
Additional errors include inappropriate code selection based on lesion type rather than procedure performed, or failing to understand the “add-on” code structure for multiple biopsies during the same session.
The Solution: Establish clear coding protocols based on procedural intent and documentation:
Biopsy coding guidelines:
- Primary purpose is tissue sampling for diagnosis
- May be punch, shave, or incisional technique
- Use 11102 for first lesion, 11103 for additional lesions
- Document technique, size of sample, and anatomical location
Excision coding guidelines:
- Complete lesion removal with therapeutic intent
- Include margin assessment and closure
- Select codes based on anatomical location and specimen size
- Document margin status and closure method

Train clinical staff to clearly document the intent of each procedure in operative notes. Implement procedure-specific templates that capture all necessary elements for appropriate code selection. Consider using clinical photography to document lesion characteristics and procedural approach.
6. Use of Non-Specific ICD-10 Diagnostic Codes
The Error: Using generic or non-specific ICD-10 diagnostic codes when more detailed codes are available can lead to claim denials due to insufficient medical necessity documentation. Payers increasingly require specific diagnostic justification for services, particularly for procedures and higher-level E/M visits.
Common errors include using unspecified codes when specific variants are documented, failing to use appropriate seventh characters for encounter types, or not coding to the highest level of specificity available in the medical record.
The Solution: Implement comprehensive ICD-10 coding practices that maximize specificity:
Best practices for diagnostic coding:
- Always use the most specific code available that accurately describes the patient’s condition
- Stay current with annual ICD-10 updates and new code additions
- Use combination codes when available to reduce the total number of codes needed
- Ensure proper sequencing with primary diagnosis first
- Document all relevant comorbidities and complications that affect treatment
Dermatology-specific considerations:
- Use anatomical site-specific codes when available
- Include laterality (right, left, bilateral) when relevant
- Code morphology and behavior of neoplasms appropriately
- Document and code all relevant clinical findings and symptoms
Provide regular ICD-10 training focusing on dermatology-specific coding scenarios. Develop diagnosis coding reference tools and decision trees for common conditions. Implement coding software that suggests the most specific available codes based on documentation.
7. Failure to Stay Current with Coding Guidelines and Payer Policy Changes
The Error: The healthcare coding landscape is constantly evolving, with annual updates to CPT and ICD-10 codes, changes in Medicare and commercial payer policies, and new regulatory requirements. Failing to stay current with these changes can result in using obsolete codes, violating payer-specific policies, or missing opportunities for improved reimbursement.
This is particularly challenging in dermatology, where new procedures, technologies, and treatment approaches frequently require new coding strategies. Additionally, payer policies for services like Mohs surgery, photodynamic therapy, and cosmetic procedures are subject to frequent changes.
The Solution: Establish a comprehensive continuing education and policy monitoring system:
Educational initiatives:
- Invest in ongoing training for coding and billing staff
- Subscribe to dermatology-specific coding publications and newsletters
- Attend relevant conferences, webinars, and training sessions
- Maintain certifications and continuing education requirements
Policy monitoring:
- Regularly review updates from major payers (Medicare, Medicaid, commercial insurers)
- Monitor changes from professional organizations like the American Academy of Dermatology
- Subscribe to coding update services and newsletters
- Implement a system for distributing policy changes to relevant staff
Implementation strategies:
- Develop internal communication channels for sharing coding updates
- Create testing and validation processes for new codes and policies
- Maintain documentation of policy changes and implementation dates
- Establish relationships with coding consultants for complex scenarios
Consider joining professional organizations and participating in online forums where coding professionals share insights and interpretations of new guidelines.
Building a Sustainable Revenue Cycle Management System
Avoiding these critical dermatology coding errors requires more than just awareness—it demands a systematic approach to revenue cycle management that includes:
Quality Assurance Programs: Implement regular internal audits to identify and correct coding patterns before they impact revenue. This includes pre-submission claim reviews, post-payment audits, and denial analysis to identify trends.
Technology Integration: Leverage coding software, electronic health records, and revenue cycle management systems that provide real-time coding assistance, compliance checks, and analytics to optimize financial performance.
Staff Training and Development: Invest in ongoing education for all staff involved in the revenue cycle, from providers documenting encounters to coders selecting appropriate codes to billing staff managing claim submission and follow-up.
Performance Monitoring: Establish key performance indicators (KPIs) such as clean claim rates, days in accounts receivable, denial rates by error type, and coding accuracy metrics to track improvement over time.
Conclusion
The complexity of dermatology coding presents both challenges and opportunities for practices committed to excellence in revenue cycle management. By addressing these seven critical error areas through systematic improvements in documentation, coding accuracy, staff training, and policy compliance, dermatology practices can significantly improve their financial performance while ensuring appropriate patient care documentation.
Remember that coding accuracy is not just about compliance—it’s about ensuring that your clinical expertise and patient care efforts are appropriately recognized and compensated. The investment in robust coding practices and ongoing education will pay dividends through improved cash flow, reduced audit risk, and enhanced practice sustainability.
The dermatology landscape will continue to evolve with new treatments, technologies, and regulatory requirements. Practices that establish strong foundational coding practices and maintain commitment to continuous improvement will be best positioned to thrive in this dynamic environment while providing excellent patient care.